The Crucial Role of Primary Care: A Closer Look at Cost Savings and Population Health Management
- Oct 31, 2023
- 3 min read
Is there substantiated evidence indicating that more frequent visits to your Primary Care Physician (PCP) can result in decreased healthcare costs for a population? Let's delve into the key strategies that MSSP ACOs employ to manage their Medicare populations, with a special focus on the role of the PCP.
One essential strategy adopted by a majority of ACOs is the completion of the Annual Wellness Visit (AWV). This visit holds immense value as it offers a dedicated time to develop preventive care plans, address gaps in care, enhance diagnosis coding accuracy, and contribute to patient attribution within the ACO network. At the heart of the wellness visit lies the opportunity to build comprehensive preventive and chronic care plans, aiming to detect diseases and conditions early while mitigating the exacerbation of chronic illnesses.
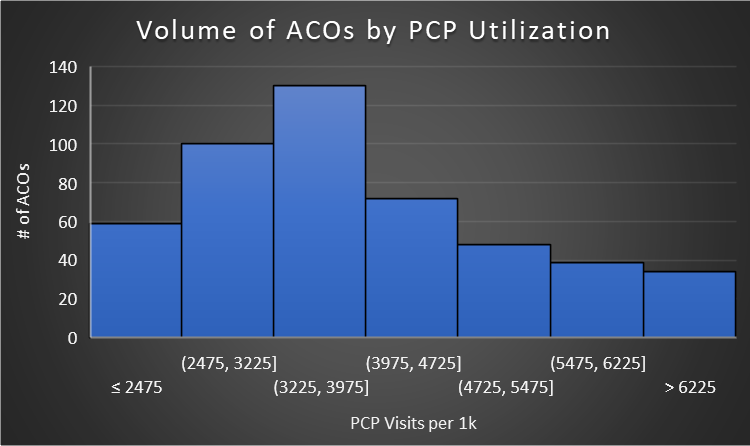
When we look at the data, ACOs, on average, record 3,910 PCP visits per 1,000 patients, translating to roughly four visits per patient each year. However, an interesting trend emerges when analyzing the 2022 performance results of MSSP ACOs – there are prominent variations in PCP utilization across different ACOs. Notably, 46 MSSP ACOs reported populations that visited their PCPs between 6 to 13 times annually per patient.
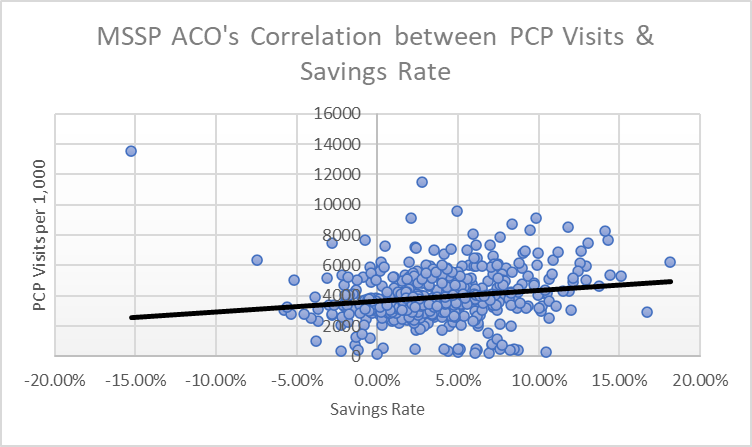
It's often referenced that the PCP plays the role of the "quarterback" in a patient's care journey, helping them navigate the complexities of the healthcare system. This prompts an intriguing question: can we infer that more frequent PCP visits result in better-coordinated care and, subsequently, improved disease management, leading to a reduction in overall medical costs? Moreover, does the available data from MSSP ACOs provide evidence to support this hypothesis? Let's explore the numbers and delve deeper into this vital topic.
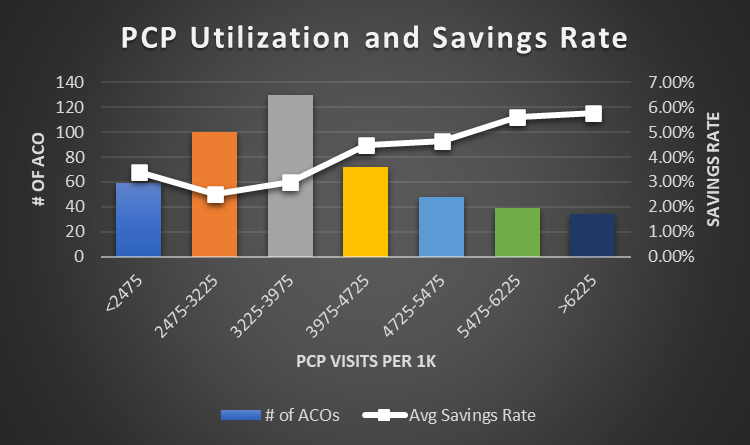
As we examine the relationship between the frequency of Primary Care Physician (PCP) visits and cost savings in healthcare, some intriguing insights come to light. It's crucial to understand what factors contribute to these savings and whether they are linked to reduced expenditures and utilization.
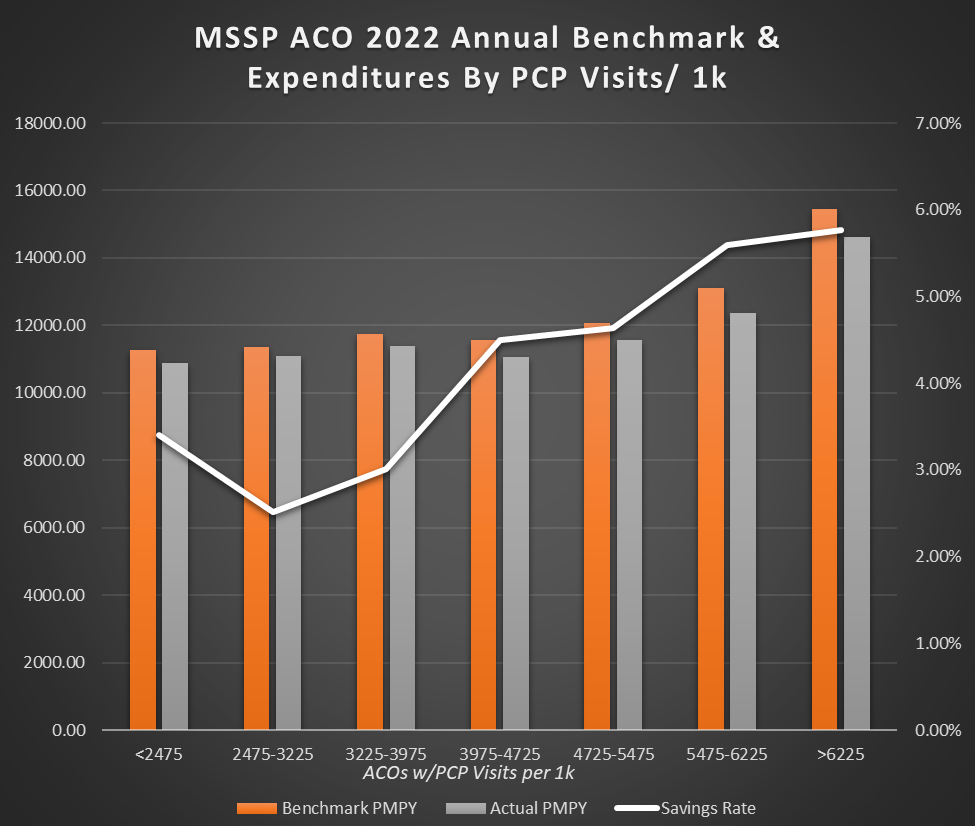
The numbers tell an interesting story. MSSP ACOs that averaged four PCP visits per year achieved a 4.5% savings rate, while those with an average of six visits generated a savings rate exceeding 5.6%. In contrast, ACOs with fewer than four visits achieved savings rates of 2-3%. This trend suggests that a higher number of PCP visits is associated with more significant savings in value-based care arrangements.
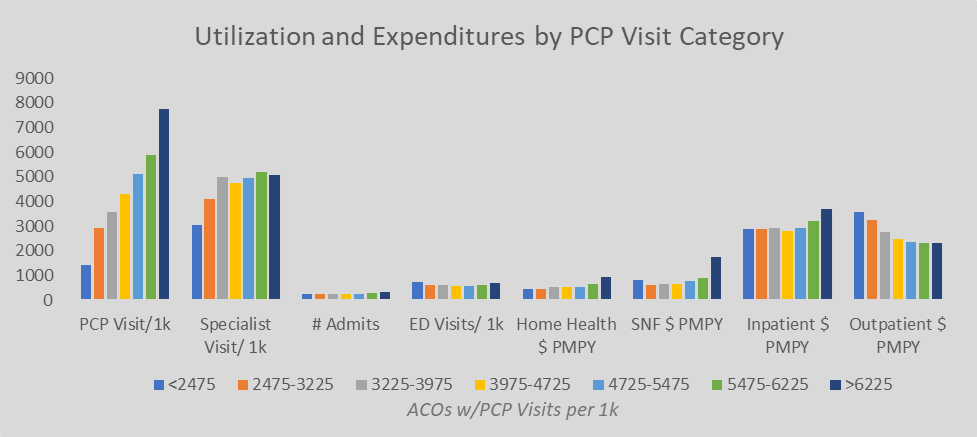
Contrary to what one might expect, across high-cost care settings, ACOs with a higher utilization of PCPs do not necessarily exhibit lower frequency or lower costs. In fact, our data reveals that ACOs with more PCP visits tend to have higher costs in several care settings, with one notable exception: outpatient services. This prompts us to consider whether ACOs with a greater number of PCP visits serve a population that faces more severe illnesses and diseases, necessitating more frequent visits.
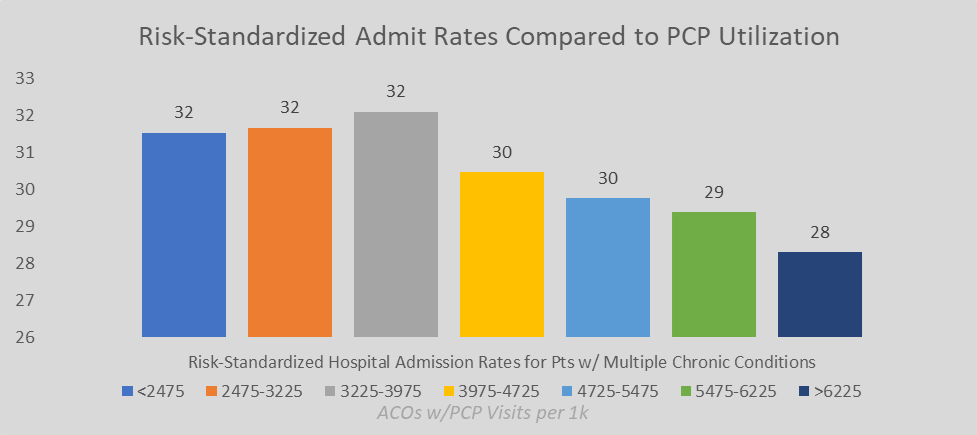
When we delve into ACO quality metrics, it's worth noting that the risk-adjusted admission rates show better outcomes for populations with more PCP visits. However, readmission rates and overall quality performance scores seem to remain consistent regardless of the number of PCP visits per 1,000 patients.
Let's take a closer look at risk factors, benchmarks, and actual total cost of care expenditures across ACOs, relative to their PCP visit rates. Populations with a greater number of PCP visits per year tend to have higher benchmark and actual expenditures compared to those with fewer visits. However, when we consider the savings rate, we find that those with more PCP visits are comparatively generate more savings. This could be attributed to the opportunity to accurately capture population risk through diagnosis coding. Still, it's essential to recognize that they are likely dealing with a higher-risk patient population, necessitating more frequent visits regardless of coding opportunities.
In summary, the data strongly suggests that an increase in PCP visits is associated with greater cost savings and indicates a population with higher healthcare risk. When conducting a comparative analysis of expenditures and utilization, it becomes evident that risk adjustment plays a pivotal role in clarifying the impact of PCPs in healthcare management. These trends underscore the fundamental importance of PCPs as the cornerstone of successful population health management.
In the continuously evolving landscape of primary care and value-based healthcare, a deep comprehension of these dynamics remains paramount. Engage with us in navigating this intricate terrain, where PCPs are pivotal in driving positive outcomes and cost-effective healthcare. #PrimaryCare #ValueBasedHealthcare #PopulationHealthManagement #MedicareSharedSavingsProgram #ACO #MSSP
PUF 2022 Medicare Shared Savings Program Performance Result Analysis
Supporting Data:


Comments